
Like all parts of our bodies, diabetes can affect the eye. The light sensitive layer inside the eye is called the retina. This tissue is composed mainly of specialized nerve tissue (rods and cones) and blood vessels.
When diabetes is poorly controlled, the blood vessels in the eye become abnormal. The abnormalities in these vessels often result in small aneurysms and hemorrhages (microaneurysms and dot-blot or flame hemorrhages). In the early stages, these changes are often asymptomatic.
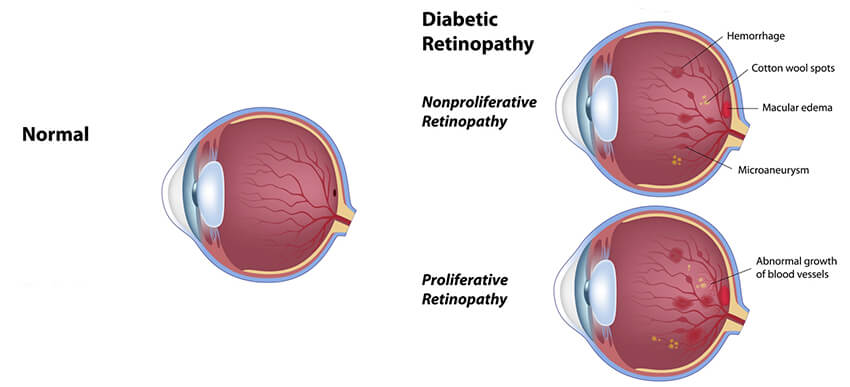
These damaged vessels are unable to adequately transport oxygen to retina, which can damage the nerve tissue – a process called retinal ischemia. Eventually, the oxygen-deprived retina releases a chemical (VEGF) that causes more blood vessels to grow. However, these vessels are not normal vessels. They tend to leak fluid, form scar tissue and can pull on the retina, causing retinal detachments.
These affects can be profound, leading to vision loss. If these changes are detected early, they are much more treatable than if they are advanced at the time of diagnosis. If you have diabetes, it is extremely important to get routine follow up with your eye doctor to detect these changes at an early stage.
In the early stages, you may not know you have diabetes. Your primary care doctor will likely instruct you to see your eye doctor as part of your overall diabetes care. However, if your blood sugars are too high for too long, you may notice some of the signs of diabetes in the eye.

Not all patients develop diabetic changes in their eyes, and often times, diabetes will have no effect on your vision. However, if you develop diabetic retinopathy, visual changes may occur. Macular edema is fluid accumulation in the part of the eye responsible for central vision. This can cause blurring that doesn’t improve, even with new glasses. With bleeding (vitreous hemorrhage) you may notice sudden increases in floaters, often times patients describe this event as suddenly seeing “ink in water”, “snow globe” or “swarm of bees.” Advanced cases can develop retinal detachments which can significantly limit vision and often requires surgery.
The best way to stop diabetes from affecting your eyes is to maintain good blood glucose control! Do you know your Hemoglobin A1c? This number is an average of the last 3 months of blood sugars. It gives your primary care doctor an idea of what your control has looked like (even with daily fluctuations). However, it also gives you a good target!
Studies have shown that an A1c of around 6 to 6.5 is ideal to prevent diabetes from developing in the eye. An A1c of 7 or more puts you at significantly increased risk for diabetes development in the eye.
The best way to prevent diabetes in the eye is to control blood sugars and blood pressure. Once diabetes becomes established in the eye, treatment centers around two problems – swelling in the macula and bad blood vessel growth (Proliferative Retinopathy).
Swelling in the back of the eye is called macular edema and can sometimes be treated with medications called VEGF inhibitors or low-intensity laser called Focal Laser. Once proliferative retinopathy occurs, the ischemic areas of the retina need to be treated. Laser treatments to the peripheral retina called panretinalphotocoagulation (PRP), treat the oxygen-deprived areas of the retina to prevent them from releasing VEGF, which prevents growth of new, harmful blood vessels.
Colorado Eye Consultants is dedicated to the preservation of sight and providing patients with the quality of life they deserve. Our patients receive personalized care by knowledgeable and experienced board certified ophthalmologists to ensure the clarity needed to see the most important things in their world. Your vision is our utmost priority and we offer same day appointments to ensure you get the care you deserve!
Request an Appointment